Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Rewrite the content and keep the original meaning and format, and add 5 more H2, the content is “
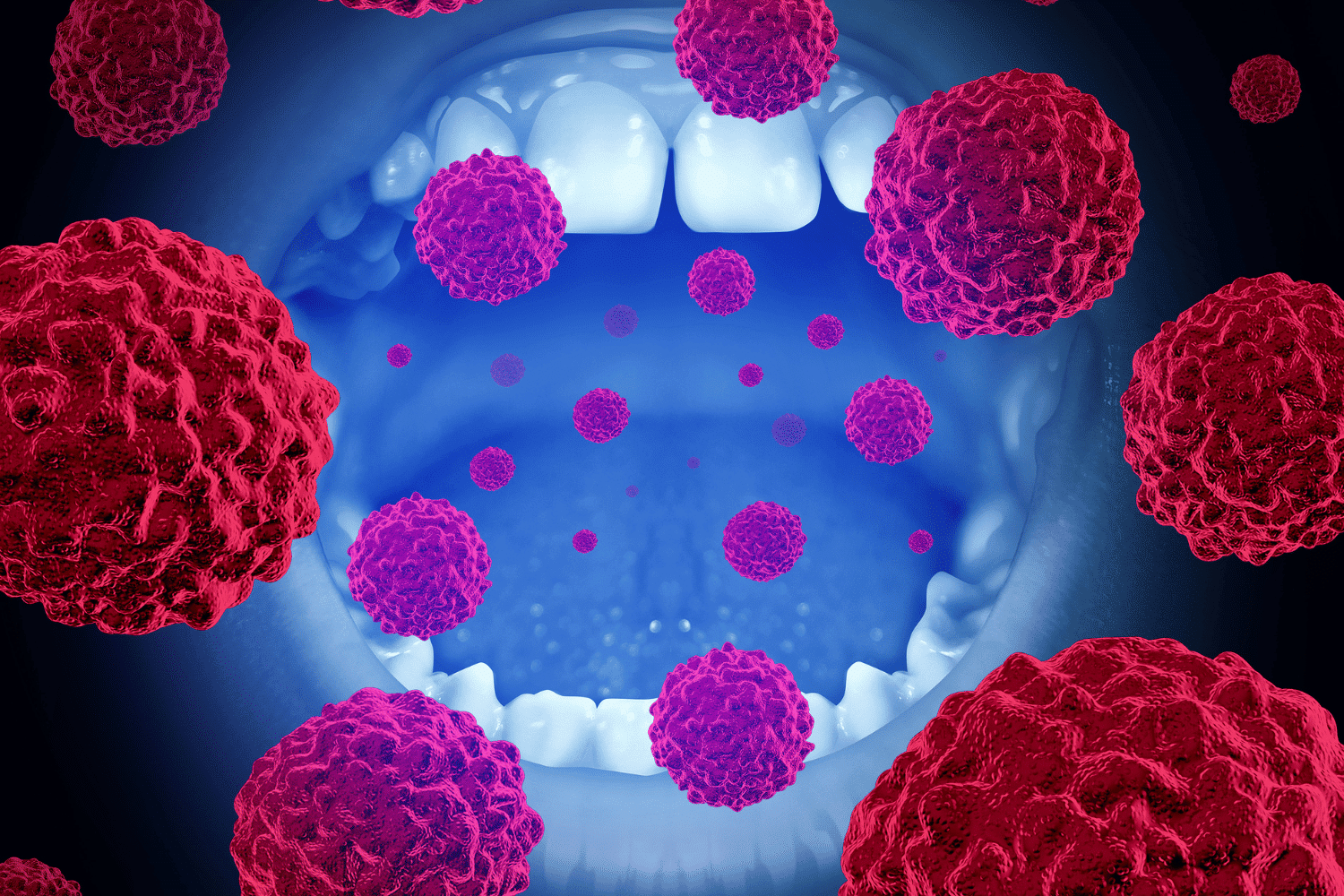
Recognizing symptoms of an oral infection, such as pain, swelling, or unusual patches in your mouth, is key to seeking timely treatment. This article will help you identify the common symptoms of an oral infection symptoms and know when it’s time to visit a dentist.


Oral infections encompass a variety of infections that occur within the mouth, affecting dental and non-dental areas alike. These infections are typically caused by an overgrowth of harmful microorganisms, including bacteria, viruses, and fungi. Factors such as age, underlying health conditions, and oral hygiene habits significantly influence the likelihood of developing oral infections.
Poor oral hygiene is a major contributor to the development of bacterial infections. When harmful bacteria proliferate due to inadequate dental care, they can lead to various issues within the oral cavity, including the gums, tongue, and throat.
Understanding these causes and influences is the first step in preventing and managing oral infections.


Several common oral infections can affect different parts of the mouth. These include dental caries, gum infections, oral thrush, and oral herpes. Dental caries, or cavities, result from tooth decay caused by bacteria that thrive on sugary foods and beverages.
Gum disease, such as gingivitis, is an early stage of periodontal disease characterized by inflammation and bleeding of the gums. If left untreated, it can progress to periodontal disease, which damages the tissues and bones supporting the teeth.
Oral thrush, a fungal infection caused by Candida albicans, is particularly common in individuals with weakened immune systems and can be triggered by antibiotic use. Oral herpes, caused by the herpes simplex virus, manifests as fluid-filled blisters that can recur throughout a person’s life and is highly contagious. Fungal infections can also pose a risk to those with compromised health.
Canker sores, though not caused by infections, are another common issue and can be triggered by stress, hormonal changes, or food sensitivities. Understanding these common oral infections helps in recognizing and addressing them promptly.
Recognizing the symptoms of mouth infections is crucial for early intervention and treatment. Common symptoms include painful sores, swelling, redness, bleeding gums, persistent bad breath, white patches, and tooth sensitivity and pain. Each of these symptoms can point to different types of oral infections, necessitating a closer look.
Painful sores, swelling, and redness often indicate an underlying infection or inflammation. Bleeding gums can be a sign of gum disease, while persistent bad breath might suggest a bacterial infection. White patches or coatings in the mouth could indicate a fungal infection like oral thrush.
Lastly, tooth sensitivity and pain can signal dental problems such as cavities or gum recession. Understanding these symptoms helps in identifying the specific type of oral infection one might be facing.
Mouth sores can arise from various causes, including infections, systemic diseases, irritation, or allergic reactions. Among these, canker sores, or aphthous ulcers, are a common type of non-infectious sore, often triggered by stress, hormonal changes, or food hypersensitivity. Unlike cold sores caused by the herpes simplex virus, canker sores are not contagious.
These ulcers often appear red or white and may be accompanied by blisters, making eating and speaking uncomfortable. The typical healing time for canker sores is about 10-14 days, but during this period, they can cause significant pain.
To alleviate the discomfort, it’s advisable to avoid acidic foods and practice gentle toothbrushing. Salt-water rinses can also provide symptomatic relief. Recognizing and managing painful sores effectively ensures they heal without further complications.
Swelling and redness in the gums or other parts of the mouth are significant indicators of an infection or gum disease. When bacteria infect the gums, it often leads to inflammation, making the gums appear red, swollen, and tender. This is particularly common in the early stages of gum disease.
In some cases, a small pimple-like swelling on the gums may indicate the presence of an abscess, which is a localized infection that requires prompt dental care. Recognizing these signs early on can help in seeking timely treatment and preventing further complications.
Bleeding gums during brushing or flossing are often a sign of inflammation caused by bacteria in dental plaque. This is typically an early indication of gum disease, such as gingivitis, which, if left untreated, can progress to more severe periodontal disease.
The accumulation of bacterial plaque due to poor oral hygiene practices is the primary cause of this inflammation. Maintaining good oral hygiene, including regular brushing and flossing, is essential to prevent gum disease and associated bleeding gums.
Chronic bad breath, or halitosis, can often be traced back to the production of gases by bacteria present in the mouth. This persistent bad breath is not just a social inconvenience but can also indicate underlying oral health problems that need to be addressed.
Poor oral hygiene can lead to an accumulation of bacteria, exacerbating bad breath. Good oral hygiene practices, including regular brushing and flossing, are crucial in preventing persistent bad breath and maintaining a healthy mouth.
White patches or coatings in the mouth are often a sign of a fungal infection, such as oral thrush. This condition is commonly caused by the overgrowth of the fungus Candida albicans. Oral thrush typically develops on the roof of the mouth or the tongue and is characterized by a whitish buildup.
Common symptoms of oral thrush include a loss of taste, a painful burning sensation, and persistent white patches. Early recognition of these symptoms can lead to appropriate treatment and prevent the infection from spreading or worsening.
Tooth sensitivity often manifests as sharp pain when consuming hot, cold, or sweet foods, indicating possible underlying dental issues. This sensitivity can be caused by dental caries, worn enamel, or gum recession, all of which expose the sensitive layers of the tooth.
Conditions such as periodontal disease or cracked teeth can also lead to tooth sensitivity and necessitate professional evaluation. Addressing these issues promptly can prevent further damage and ensure a healthy mouth.
Recognizing symptoms of oral infections is critical for seeking dental care promptly. Persistent tooth pain, swelling, and bad breath, even after maintaining good hygiene practices, are signs that require immediate dental consultation. Early diagnosis and treatment of oral infections lead to a good prognosis, preventing complications and ensuring oral health.
Regular dental visits are crucial for the early detection and management of oral health issues, thereby preventing infections. Treatments for oral infections may involve procedures like draining abscesses and administering antibiotics.


Today’s Dental employs advanced technology, to create surgical guides that enhance precision in the treatment of complex oral infections. Understanding the effective treatment options available for oral infections is critical for ensuring patient health and comfort.
Treatment approaches vary depending on the type and severity of the infection. From medical treatments to home remedies and preventive care, each option plays a crucial role in managing oral health effectively.
Available treatments for mouth infections include antibiotics, antivirals, and antifungals. For severe dental infections with systemic symptoms, intravenous antibiotics may be required. Clindamycin is often used for patients allergic to penicillins or cephalosporins in treating oral infections.
The choice of antibiotics for dental abscesses may depend on local resistance patterns. Oral thrush is treated with medical antifungal medications, including topical antifungal ointments or antifungal mouthwash. Antiviral medications are used for oral herpes, although there is currently no cure for this condition.
Salt-water rinses can provide symptomatic relief for mouth sores. Home remedies may help to alleviate symptoms of oral infections and improve overall comfort. Maintaining good oral hygiene practices, such as regular brushing and flossing, is essential to prevent oral infections.
Incorporating home remedies with preventive care measures can enhance oral health and mitigate symptoms of infections. Preventive care, including regular dental check-ups and a healthy diet, plays a vital role in maintaining gums and teeth while helping to prevent oral infections.


Maintaining good oral hygiene is crucial in preventing oral infections. Regular dental check-ups are essential for early detection and treatment of potential oral infections. By brushing twice daily and flossing, you can eliminate plaque and reduce the risk of infections.
Avoiding sugary foods and beverages can significantly lower the chances of developing oral diseases. Additionally, drinking fluoridated water and using fluoride toothpaste can strengthen teeth and help prevent cavities. Quitting tobacco products is also important as they increase the risk of oral infections and cancers.


In summary, recognizing the symptoms of oral infections early and seeking prompt treatment can prevent minor issues from escalating into significant health problems. Understanding the common types of oral infections and their symptoms is crucial for effective management and treatment. Regular dental visits and good oral hygiene practices are key preventive measures that can help maintain a healthy mouth.
We at Today’s Dental are dedicated to providing top-notch care for all your dental needs. Our advanced technology, compassionate staff, and comprehensive treatment options ensure that you receive the best possible care. Prioritizing your oral health is essential for overall well-being, and we are here to support you every step of the way.
Common symptoms of oral infections include painful sores, swelling, redness, bleeding gums, persistent bad breath, white patches, and tooth sensitivity or pain. If you experience these symptoms, it’s important to seek dental care promptly.
You should seek professional dental care for an oral infection if you have persistent tooth pain, swelling, or bad breath that does not improve with good oral hygiene, or if your symptoms worsen. Prompt treatment is essential to prevent complications.
The most effective treatment options for oral infections include medical treatments such as antibiotics, antivirals, or antifungals, alongside home remedies and preventive care measures. Choosing the right approach depends on the type of infection and individual health needs.
To prevent oral infections, maintain good oral hygiene, limit sugary foods and beverages, drink fluoridated water, and avoid tobacco products. Regular dental check-ups are also essential for early detection and prevention.
Today’s Dental boasts an impressive average rating of 4.8 out of 5 stars from customer reviews. This high rating reflects a strong level of satisfaction among patients.
”